Fitting the pieces together: Completing the big picture puzzle of a coherent end-of-life care system for all
A blog post written by Dr Chris Moy, General Practitioner, Parkside, SA
A fundamental aspect of palliative care is that it is supposed to be “holistic care”. At an individual level, this emphasises the requirement to not only consider the many medical and practical aspects of a person’s care, but to also consider their emotional, social and spiritual needs.
At the level of policy and service development, this means being able to identify the many pieces of the puzzle that are required to support good end-of-life care for individuals, and to wisely fit these together so that the picture begins to make sense to everyone.
In South Australia, there has been steady progress in this regard, with the work of many individuals and organisations being the essential pieces that coming together to form a picture of a coherent end-of-life decision-making and care strategy which will better provide for the needs of people dying both in hospitals and in the community.
So, what are some of these “pieces”, and how do they fit together? Firstly, the Advance Care Directives Act 2013 and Amendments to the Consent to Medical Treatment and Palliative Care Act 1995 have given greater clarity in regards to the legal basis of end-of-life decision-making and care. There is now a single form, the Advance Care Directive (ACD), on which individuals can appoint Substitute Decision-makers (SDMs) and document wishes, instructions and “binding refusals”. The fundamental basis on which others must decide when the individual loses decision-making capacity is now clear- we must genuinely try to do as they would have wanted and to decide “as if in their shoes”.
There is clarity in regard to the hierarchy of individuals or documents that health practitioners must consult in obtaining consent for treatment: an SDM first, followed by relevant instructions on an ACD, followed by a legally defined group of individuals known as “Persons Responsible”. And the legislation supports good end-of-life care in making it clear that medical practitioners should not have to provide treatment that is of no medical benefit (some call this “futile treatment”) to a dying patient, and that they will be protected in the provision of medication that is adequate in maintaining the comfort and dignity of their patient, even if this may have a secondary effect of shortening their life.
A second “piece” of the puzzle was driven out of the understanding that while an ACD is important in protecting the wishes of an individual, it may not convey clear enough instructions to be useful if they rapidly decline, or suffer a cardiac arrest, and urgent decisions about resuscitation need to be made. The Resuscitation Plan-7 Step Pathway is a clinical plan that is completed by the doctor responsible for the individual’s care, and requires the doctor to go through seven logical steps in making decisions about resuscitation and end-of-life care, that align with their legal (including ACD and Consent Acts), ethical, and professional responsibilities. Of paramount importance, the Resuscitation Plan asks this essential question: “If the patient is not for resuscitation or curative care, what are you going to do to ensure the comfort and dignity of your patient?” And the aim of standardisation of use and recognition of this form by all sectors – hospitals, ambulance service, general practice, community and aged care- increases the chance that clinical instructions aligning with the person’s wishes are actually carried out, including attempts to maintain an individual in their home, if that is their wish. Note that a “Community Version” of this form is due for release soon.
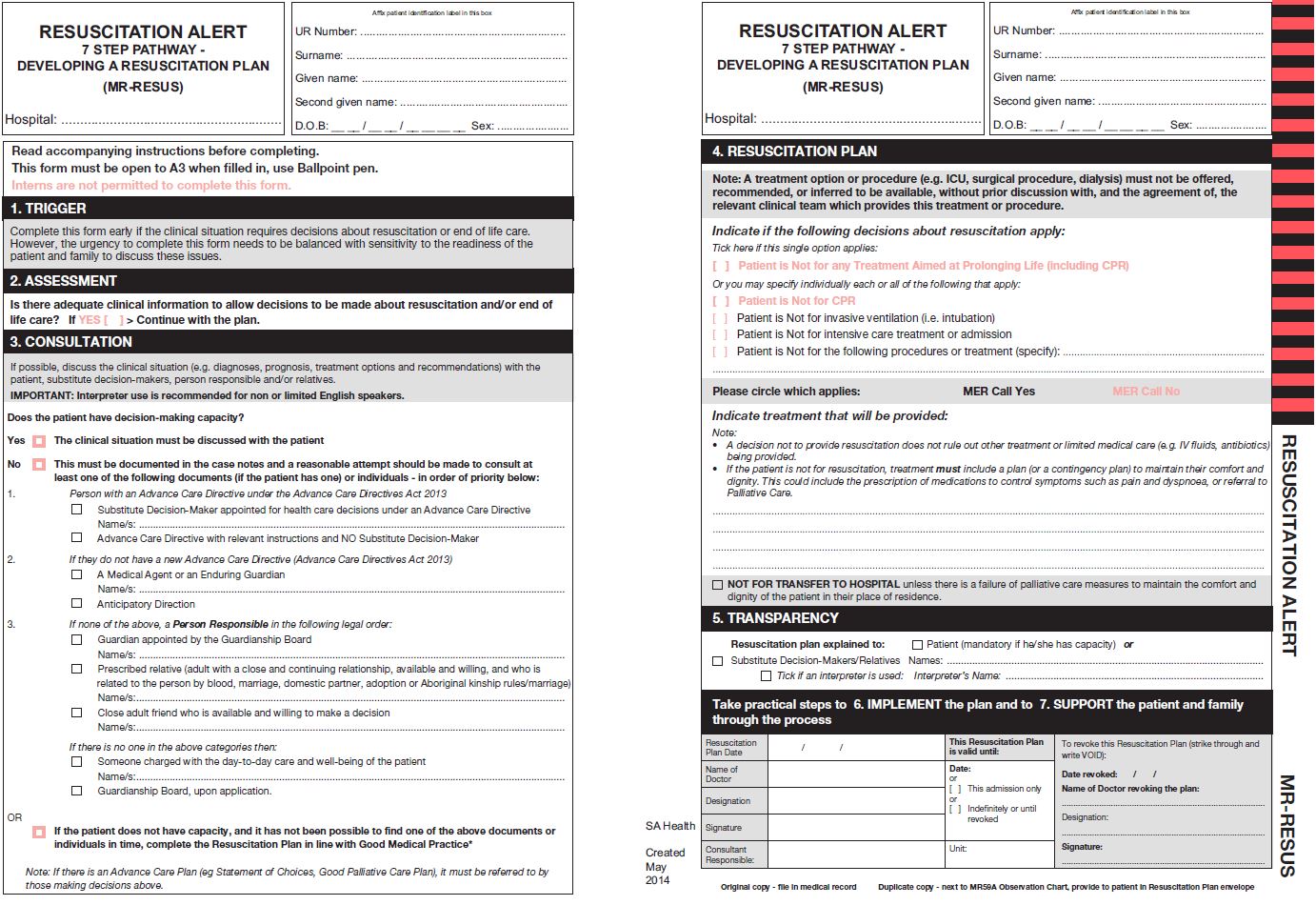
(click image to view a larger version in a new window)
But to be of any use in the common situation of an emergency, how will it be possible to get these documents to the point of care? Within SA Health, one of the system integration initiatives in this endeavour has been a change to admission procedures to request for, and to upload, patient ACDs and Resuscitation Plans onto electronic records, as well as moving away from asking for “next of kin” to asking for the individuals who can legally consent on behalf of patients: “Substitute Decision-makers” and “Persons Responsible”. On a national level, there appears to be progress in moves to allow the upload of ACDs onto a patient’s electronic health record- the unfairly maligned PCEHR- which will allow any health practitioner to view these documents for a patient when they are most needed anywhere across Australia.
And what about the actual provision of end-of-life care to dying people? So much is happening, including:
- The finalisation and endorsement under Transforming Health of a standard Specialist Palliative Care Service Model of Care, that was developed by the SA Health Palliative Care Clinical Network Steering Committee chaired by Ms Kate Swetenham, so that there is fairness and equity in regard to the provision of a comprehensive service to provide for the medical, practical and psychosocial needs of individuals across the state.
- Efforts to clearly embed standardised triggers to initiate end-of-life discussions with patients within SA Health, coupled with upskilling in end-of-life care provision, so that all health practitioners, not only palliative care specialists, can better provide this for their patients.
- The successful trialling of an End of Life Clinical Lead model –Dr Christine Drummond- in the Northern Adelaide Health Service. With a role analogous to an Infection Control Officer in the implementation of infection control strategies, this role has supported the implementation of the ACD and Resuscitation Plan-7 Step Pathway and, more importantly, fostered a clear improvement in the culture and skills of all staff in regards to the end-of-life care of patients- bringing closer the dream of “making end-of-life care everybody’s business.”
- The introduction of the GP Palliative Care Shared Care Program by SA Health and administered by GP Partners Australia.
This aims to upskill GPs in palliative care skills while working in partnership with the Specialist Palliative Care
Service to reduce the gaps in care that exist between the silos in the healthcare system, and which
sometimes lead patients and their families to feel abandoned when they most need help.
- The finalisation of the SA Health Prescribing Guidelines for the Pharmacological Management of Symptoms for Adults in the Last Days of Life, a two page guideline outlining simple recommended initial medications, doses, and administration regimens for the management of common symptoms that patients may suffer in the last days of life.
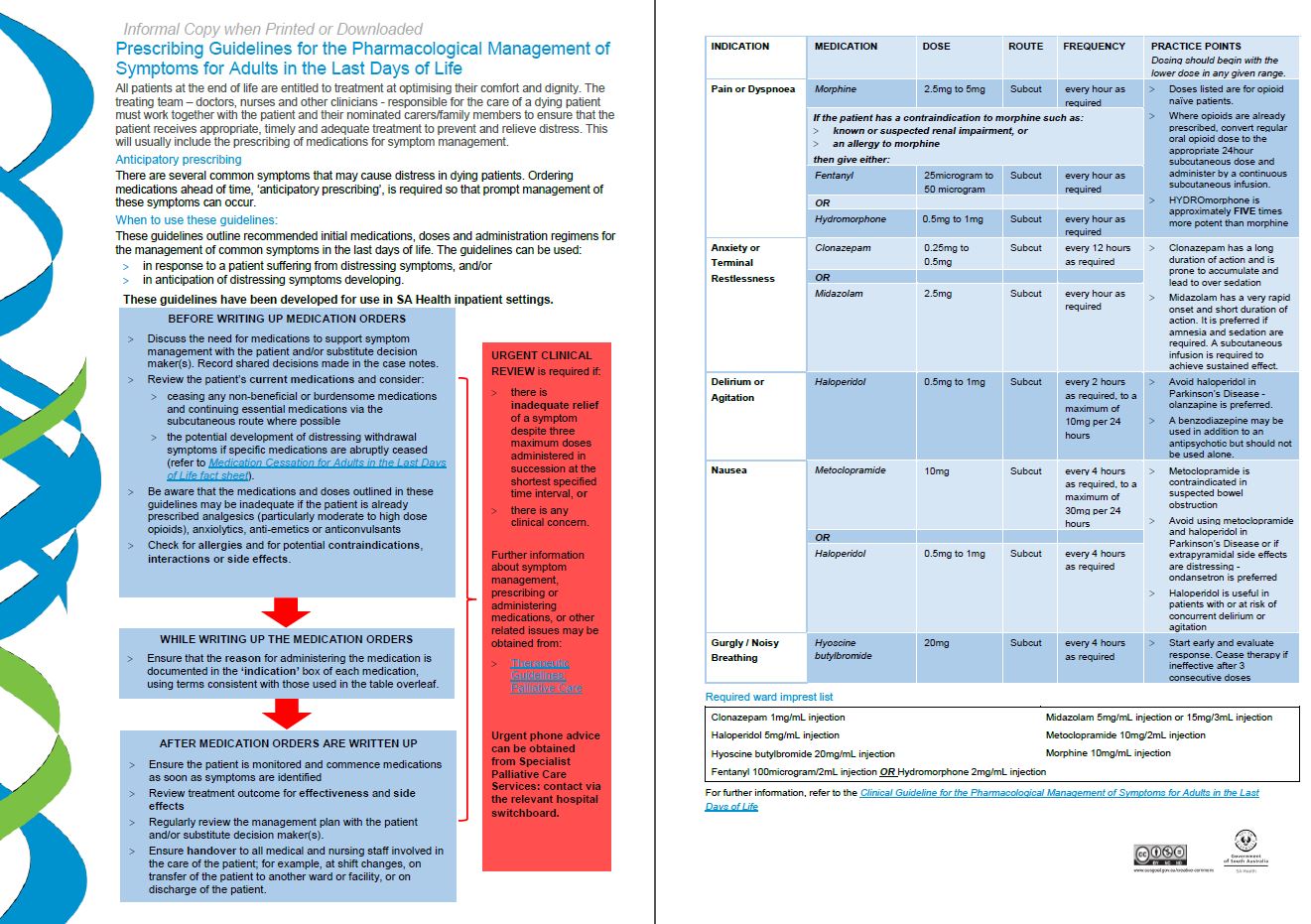
(click image to view a larger version in a new window)
This provides standardised guidelines to initiate these medications, particularly aimed at doctors unfamiliar in doing so, across the state. It provides options for doctors needing to answer the practical question posed on the Resuscitation Plan- 7 Step Pathway: “If the patient is not for resuscitation or curative care, what are you going to do to ensure the comfort and dignity of the patient?”, and it follows on nicely from the work of Mr Paul Tait in developing the Core Palliative Medicines List which aims to make available the basic palliative medications that are required, at the point of care.
- Early work by the Adelaide Primary Health Network and Country SA Primary Health Network in beginning the logical broadening of implementation of many of the above initiatives into primary and aged care.
Finally, the leadership shown by the Minister for Health, Hon. Jack Snelling, MP, in setting up the End of Life Ministerial Advisory Committee, chaired by Mr Martyn Evans, is hopefully to lead to a report by the Committee laying out a clear overall strategy- the “whole picture” which the pieces of the puzzle which we have created, or will need to create, need to complete.
There is still much to do. But, if all of us working in this area can keep on identifying the missing pieces and work to create them, we can continue on the journey to build a system of care which genuinely supports the goal of holistic end-of-life care for all.
To learn more, please see:

Dr Chris Moy is a GP with Arkaba Medical Centre in Parkside, SA, as well as a member
of the SA Health Resuscitation Planning Advisory Group and former member of the SA
Health End of Life Project Working Group and the Expert Advisory Panel of the Advance
Directives Review.